Background
For decades, CML has been considered to be a triphasic disease recognizing 3 distinct stages: chronic phase (CP), accelerated phase (AP), and blast crisis (BC). Since the discovery of TKIs, the prognosis of CML patients has rapidly improved and less than 10% of patients diagnosed in CP experience disease progression on the therapy. Based on low incidence of CML progression and the fact that CML biological behavior seems biphasic, the new WHO 2022 classification of CML deemed AP less relevant and suggested the omission of AP. Many experts, however, still advocate for its inclusion in CML classification (e.g. ELN 2020, ICC 2022, NCCN 2023), even though the universal definition of AP is not established and differs in between publications.
Methods
This retrospective, real-world study is based on the Czech nationwide CML registry INFINITY with the data of newly diagnosed CML patients who agreed and provided their written consent. Recruited subjects were adult patients diagnosed in years 2005 - 2022 with sufficient data to determine the phase of the disease at diagnosis and follow-ups to assess their overall survival (OS), disease specific survival (DSS) and progression-free survival (PFS). The phase of the disease at the time of diagnosis was determined using the classification according to ELN 2020, ICC 2022, WHO 2016, and WHO 2022. Whenever CP was established, EUTOS Long-Term Survival (ELTS) score was calculated, assigning the patient to low risk (LR), intermediate risk (IR) and high risk (HR) group. OS and PFS are defined according to published guidelines. DSS is defined as the time from diagnosis to death due to CML disease or CML treatment.
Results
During the studied time period, 1660 new cases of CML were reported in INIFINITY registry. Of them, 1500 patients had data sufficient to classify the phase of the disease at the time of the diagnosis according to ELN 2020 guidelines and WHO 2022 classification and 1395 patients had data to assess the phase according to WHO 2016 and ICC 2022 classifications.
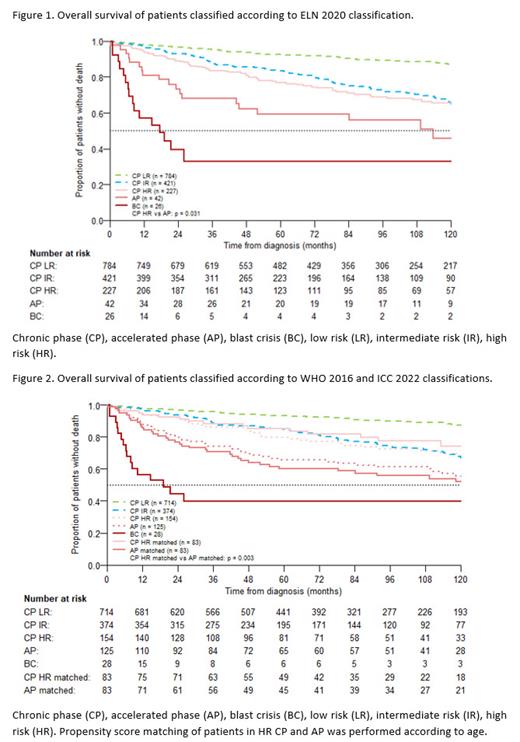
When using ELN 2020 guidelines, groups were assigned as follows: LR CP- 784 patients (52.3%), IR CP- 421 patients (28.1%), HR CP- 227 patients (15.1%), AP- 42 patients (2.8%), BC- 26 patients (1.7%). There were significant differences in representation by gender, age, comorbidities and performance score amongst patient groups. When comparing just HR CP and AP CML patients, there were no significant differences. Calculated estimates of 5- and 10- year OS, respectively, were 92.5% and 87.2% for LR CP, 83.5% and 65.9% for IR CP, 76.9% and 65.5% for HR CP, 59.2% and 45.9% for AP, and 32.9% for BC, p= 0.031 for HR CP versus AP (Figure 1).
In the case of WHO 2016 and ICC 2022 classifications, 714 (51.2%) patients were diagnosed in LR CP, 374 (26.8%) in IR CP, 154 (11.0%) in HR CP, 125 (9.0%) in AP, and 28 (2.0%) in BC. Again, there were significant differences in representation by gender, age, comorbidities and performance score amongst patient groups. When comparing just HR CP and AP CML patients, only age at the time of diagnosis was significantly different. Calculated estimates of 5- and 10- year OS, respectively, were 93.2% and 87.5% for LR CP, 84.9% and 67.7% for IR CP, 80.0% and 69.5% for HR CP, 65.7% and 55.6% for AP, and 39.7% for BC. We also performed propensity score matching according to age for patients in HR CP and AP and calculated estimates of 5- and 10- year OS, respectively, were 85.4% and 74.4% for HR CP and 60.2%, and 52.0% for AP, p= 0.003 (Figure 2).
Similar results were obtained when testing for PFS and DSS.
Summary
Real-world data obtained from 1500 patients diagnosed in Czechia over 17 years, in our opinion, support the need to recognize the existence of AP at the time of diagnosis, even though a singular definition of AP is not agreed upon. Patients in AP have worse survival scores (OS, DSS, PFS) compared to patients in CP and/or HR CP. Moreover, because ELTS risk score was calculated on patients in CP, it may not be suitable for patients in AP, which would be changed to CP according to the new WHO 2022 classification. In conclusion, based on the real-world data with long-term follow-up, we believe it would be reasonable to keep the AP as part of CML classification of newly diagnosed patients.
This publication was supported by the grant number MUNI/A/1224/2022, Programme EXCELES, ID Project No. LX22NPO5102, and by the Ministry of Health of the Czech Republic grant number 00023736.
Disclosures
Hornak:Novartis: Consultancy, Other: travel grant, Speakers Bureau; Angelini Pharma: Consultancy. Mayer:BeiGene: Research Funding. Faber:Zentiva: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Angelini Pharma: Honoraria, Speakers Bureau. Jindra:Takeda: Membership on an entity's Board of Directors or advisory committees; Roche: Honoraria, Speakers Bureau; AstraZeneca: Honoraria, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees. Zackova:Pfizer: Honoraria, Other: travel grant, Speakers Bureau; Astra Zeneca: Other: travel grant; Novartis: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: travel grant, Speakers Bureau; Angelini Pharma: Consultancy, Honoraria, Other: travel grant, Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal